Britons spending thousands on controversial therapy to tackle antibiotic-resistant infections
Desperate Britons are spending thousands on a controversial bacteria-busting medical treatment in overseas clinics as more and more succumb to drug-resistant infections.
It comes as MPs last week urged the government to commit more funding for research into the treatment, known as bacteriophage – or phage – therapy, amid growing concerns over the threat posed by antimicrobial resistance (AMR).
According to the World Health Organisation, AMR kills 4.9 million every year globally, and it’s estimated this number will rise to 10 million by 2050 as viruses, bacteria and other pathogens further evolve to evade modern medicine – driven by the excessive use of antibiotics and antivirals.
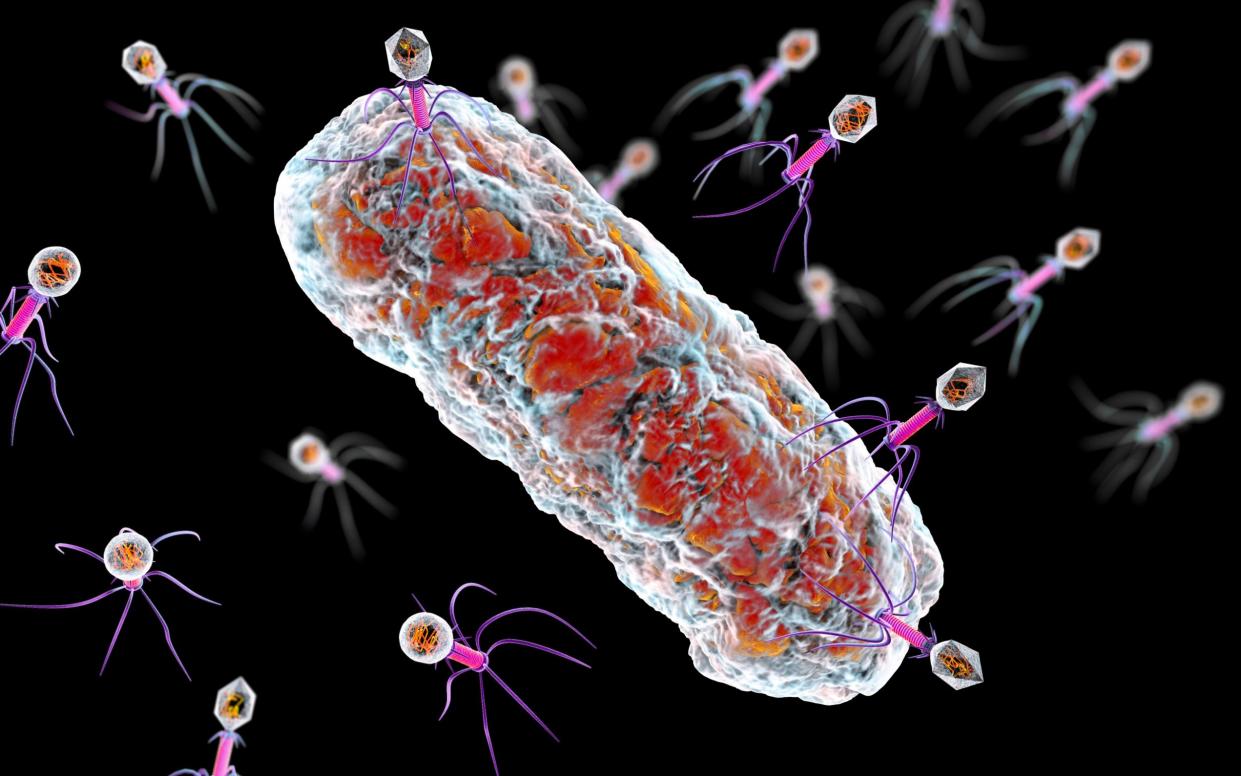
Phage therapy, which uses viruses that specifically target and kill bacteria, has long been touted as a potential treatment for drug-resistant infections but is not currently licensed in the UK and many other Western nations.
Its use divides the scientific community. Advocates say it offers a safe and legitimate alternative to antibiotics. Others are sceptical.
“Phage therapy is something you give to your mother-in-law, not your mother,” said Dr Simon Clarke, a microbiologist at the University of Reading.

Although not widely available in the UK, phage therapy is practised in parts of Eastern Europe. Every year hundreds of Britons suffering from long-term drug-resistant infections travel to these nations for treatment.
Clinics in Poland, Russia, and Georgia all offer services for international patients, the latter being a global hotspot. In Tbilisi, the capital, three facilities treat thousands a year – either in person or remotely, whereby patients send samples via post and are sent back the phages to take orally.
Facebook support groups are filled with Britons seeking advice on the treatment, which can cost up to £8,000 – depending on the type and length of therapy the patients receive.
Caroline Sampson, 60, who lives with an antibiotic-resistant UTI, is one of the many people who sought remote treatment from a clinic in Georgia.
She came across phage therapy on a Facebook support group. She spent £2,000 on treatment before deciding to stop.
“I was getting awful reactions, and nobody monitors you. The facility in Georgia makes it very clear they are an outpatient clinic, so if you have a nasty reaction you are on your own. It was terrifying,” she said.
“I was desperate to get better and so that’s why I tried it.
“But it was like I’d been hit by a bus. I felt completely bulldozed and very dizzy, I remember trying to have a conversation with my husband and I couldn’t even see straight.”
Others have had more positive experiences.
Simon Jones, 51, travelled to Tbilisi for treatment in 2017. Mr Jones suffered from an antibiotic-resistant UTI, which developed into prostatitis. After undergoing blood, urine, and other tests to pinpoint the bacteria behind the symptoms, he was given a course of oral phages.
After spending a total of £7,000, Mr Jones managed to successfully get rid of the infection. “If it wasn’t for the phage treatment, I wouldn’t be here today,” he said.
Britons seek advice through social media
Members of the Facebook group ‘Chronic UTI Women’s Support Group,’ which is followed by 4,000 people, appear similarly divided.
“I tried it, it was the best thing for me. It got rid of my urethral burning that I had for 9 years and no short-term antibiotics ever touched that symptom. I went to [The Elivia Phage Therapy Center] in Georgia and paid £3,350,” commented one patient on the group.
“I had a custom-made phage shipped to me from Elivia last summer, it took many months to get here and was very expensive. Unfortunately, it did nothing to clear [my infection],” said another patient.
Proponents of the medical treatment argue that, in the UK, the treatments would undergo rigorous testing to meet British pharmaceutical standards, and would benefit from the country’s world-leading microbiology labs – allowing experts to better tailor phages to patient’s infections.
“The thing about the Georgian treatments is that it is hard to say definitively how effective or safe they are, as controlled clinical trials have not been performed,” explained Dr Jason Clark, Chief Scientific Officer at NexaBiome, a phage therapy research company based in Glasgow.
“The Georgians do not operate to the same standards that we would in the UK, so product consistency is an issue. Any phage-based licensed medicine in the UK would need to go through clinical trials, and be produced to the highest manufacturing standards.”
Dr Clark added that phages are “completely safe” if they are “pure and properly characterised.”
Just last week, MPs from the Science, Innovation, and Technology Select Committee called upon the government to direct funds and research capacity into potentially rolling phage therapy out across Britain to help tackle the growing threat of antimicrobial resistance.
The report argued that the lack of regulation around phages in the UK is “irrational and discriminatory,” preventing very ill patients from accessing a therapy allowed in other countries.
Greg Clark MP, Chair of the Committee, said: “The development of phage therapies is at an impasse, in which clinical trials need new advanced manufacturing plants, but investment requires clinical trials to have demonstrated efficacy.”
Phages naturally occur in the environment and are estimated to kill 20 per cent of the world’s bacteria every day – meaning they play a significant role in the global ecosystem.
These viruses infect bacteria by attaching to their surface and injecting a genetic material which breaks down the host. In medicine, ‘custom’ phages can be genetically engineered to attack specific types of bacteria causing infection inside the human body.
‘People think it’s the new penicillin’
Commenting on the MPs’ report, Professor Martha Clokie, director of the Centre for Phage Research at the University of Leicester, said: “The UK is facing a real crisis with increasing numbers of patients dying from bacterial infections that can’t be treated.
“Ultimately [phage therapy] should result in the saving of a significant number of lives, reduce misery and suffering from chronic infections, and save the NHS considerable resources.”
However, Dr Clarke, the microbiologist at the University of Reading, said: “People think it’s the new penicillin – but it’s not.
“Phages stimulate a patient’s immune system, potentially tipping them into septic shock. Bacteria can also develop resistance to them easily, meaning that these new, expensive treatments might become useless pretty quickly – so the widespread use of phage could lead to even more antibiotic-resistant infections.”
Dr Clarke suggested there are other more efficient strategies to turn the tide on drug-resistant bacteria.
“For example, while the development of new antibiotics is slow, combining drugs that we already have has shown some effectiveness and there has been progress in developing drugs that block resistance when it’s encountered,” he said.
“We need to combine strategies like these with more traditional hunts for new antibiotics and vaccine development, to turn the tide on antimicrobial resistance.”
Last week, scientists announced the discovery of a new class of antibiotic that appears to kill one of three bacteria considered to pose the biggest threat to human health.
Zosurabalpin was found to beat highly drug-resistant strains of Carbapenem-resistant Acinetobacter baumannii (Crab) in tests on mice. It is now being tested on humans.
Protect yourself and your family by learning more about Global Health Security


