How the coronavirus crisis is set to squeeze financially strapped docs and hospitals
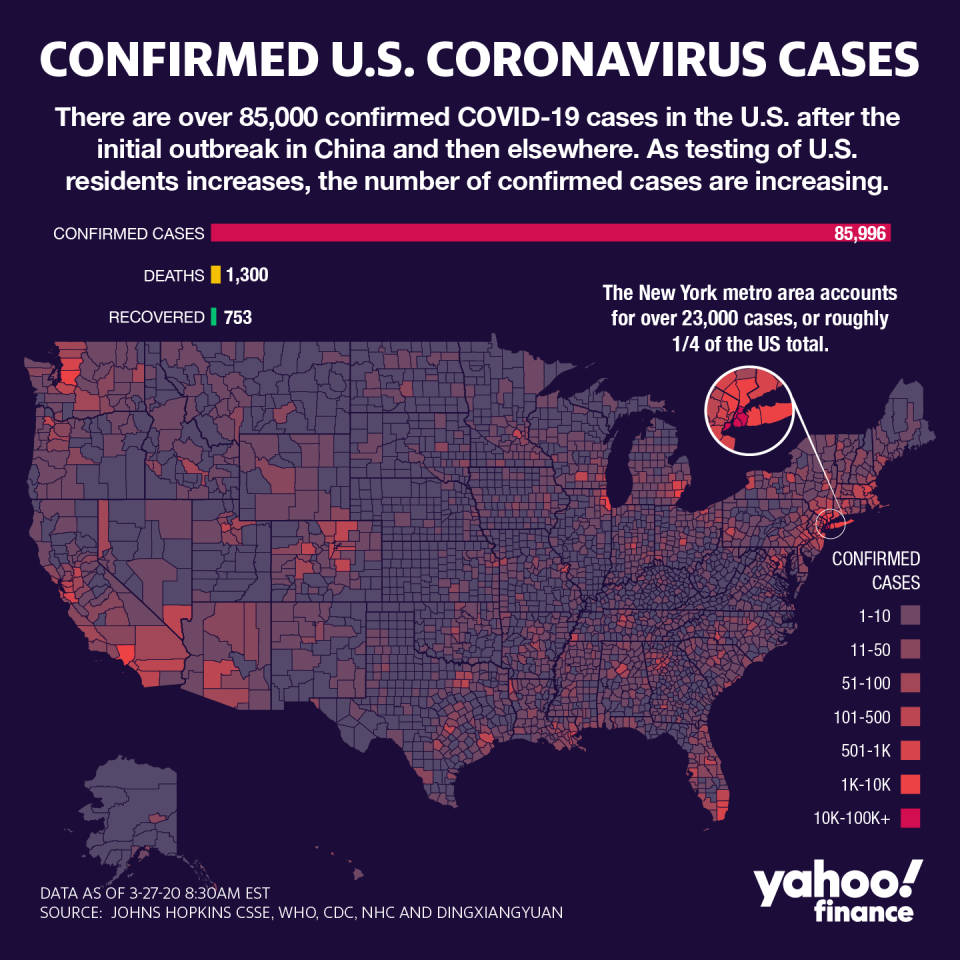
Health care is on the frontlines of managing the response to coronavirus outbreak, with efforts that range from finding effective treatments and vaccines to hospital patient care.
But those efforts are paired with a lot of uncertainty about the financial payoff. Pharmaceutical companies, hospitals and clinical labs are grappling with the cost of responding to the call of holding back the rising tide of COVID-19 infections versus the revenue they will generate. Meanwhile, physician practices may see their businesses dry up.
Which is why health care experts say the $2 trillion stimulus package that cleared the Senate late Wednesday is crucial. It includes more than $100 billion for hospitals, funding for vaccine and treatment research, and funding for a number of other health facilities.
However, a few observers see flaws: The bill helps hospitals and pharmaceuticals companies, but does not include laboratories and independent physicians.
“We need to make sure that the package also contains support for those in the private practice, those practices that are, in fact, the small businesses in their communities and pay rent and pay salaries,” Dr. Patrice Harris, president of the American Medical Association, told Yahoo Finance in an interview.
The AMA, along with the American Clinical Laboratory Association, are looking to address that gap — the latter having unsuccessfully lobbied Congress to be included in the stimulus package.
“For the third time, Congress has failed to provide the necessary funds to support ‘free testing’ for all Americans,” the group said in a statement Wednesday.
Additionally, a number of hospitals are shutting down elective surgery and similar revenue-generating business to free-up space for a potential surge, forcing those running on thin margins to face potentially hard choices about future operations. The situation has made some rural hospitals have to decide whether or not to shut down.
In fact, Moody’s recently downgraded the hospital sector from stable to negative within a week, given an expected decline in earnings for the next 12-18 months.
"The negative outlook for the US for-profit hospital sector reflects [earnings before interest, taxes, depreciation and amortization] contraction in the low-to-mid single-digits over the coming year or so, down from our previous forecast of 3% to 4% growth," said Moody’s senior credit officer, Jonathan Kanarek.
“Infections among staff may also force hospitals to bring in contract labor at higher costs, while sourcing scarce supplies may require them to use vendors they don't typically buy from, often at a greater cost,” he added.
The cost of increased staffing — which is in high demand — and additional cost of medical gear pale in comparison to the sheer volume of patients that hospitals are likely to screen as the pandemic slams the U.S.
The uncertainty is being heightened by a lack of clarity surrounding how COVID-19 claims will be categorized. Hospitals could a specific classification for coronavirus, or may code it as traditional pneumonia — all of which may affect what reimbursements will look like.
Getting squeezed on ‘bread and butter’ clients
While hospitals are preparing for the increase in Covid-19 patients, physician practices are facing the opposite as revenues get squeezed.
Dr. Farzad Mostashari, CEO of Aledade, told Yahoo Finance the outbreak is already pressuring practices where it will hurt the most: Chronic illness cases and elderly patients.
“Elderly and chronic patients are the bread and butter of primary care practices, who are, for their safety, being told to stay home and not come into the office,” he said.
Some physicians have pivoted to telehealth, something Mostashari believes won’t compensate for the financial hit resulting from losing in-person patient visits.
“The reimbursement rates [of telehealth] are about 30% less than face-to-face,” he added.
John Fanburg, health chair at the law firm of Brach Eichler, said his clients are looking at a range of strategies. Some are considering temporarily lowering staffing levels, shutting down entirely, or requesting landlords for assistance in deferring lease rents.
Either way, it delays care for the neediest patients.
“It is a very complicated business arrangement because it's not like regular retail," Fanburg said.
Some practices could qualify for a Small Business Administration loan, but that still adds a strain as the loan would have to be repaid.
The AMA announced Friday a new loan product within the SBA was launched, providing providers with fewer than 500 employees access to loans of up to $10 million. In addition, up to $100 billion from the Public Health and Social Services Emergency Fund to cover treatments related to the outbreak, as well as “on those who lose revenue due reductions in other services as a result of the pandemic. Exact eligibility criteria and application process is not yet defined pending implementation.”
Why labs matter
According to the ACLA, funding matters because a number of labs have quickly ramped up operations in response to the outbreak, and are now facing dire financial straits.
“Laboratories perform testing first, and worry about being paid later. They are still waiting for reimbursement for tests performed,” the group said, adding that many places are “burdened” with costs associated with processing specimens that don’t have all the insurance info.
“This is happening at drive thru sites across the country. The strain on laboratories is also coming at a time when the industry has endured year-over-year cuts to Medicare reimbursement to common lab tests,” the ACLA said.
Yet the uncertainty surrounding payments is nothing new, according to Dr. Howard Forman, a health economist and professor at the Yale School of Medicine.
“We never know what we will get paid for a patient coming in. A large number of patients are unable to pay after the fact This is the business,” he told Yahoo Finance.
“That’s why outpatient is where money is. With private insurance, we know how much (is being paid) and who is paying,” he added.
Free testing is being reimbursed by insurers, employers and government payors alike. The insurance industry has largely committed to covering testing and related visits, as well as select telemedicine screenings and waiving pre-authorization to move patients through hospital settings.
The industry trade group, America’s Health Insurance Providers, penned a letter to Congress warning of a need to mitigate the impact of these actions. Specifically, insurers have said premiums are likely to spike following the outbreak.
Anjalee Khemlani is a reporter at Yahoo Finance. Follow her on Twitter: @AnjKhem
Read the latest financial and business news from Yahoo Finance
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, SmartNews, LinkedIn, YouTube, and reddit.
