Hospital staffs ‘are dreading’ what’s coming as coronavirus pandemic in U.S. enters uncharted territory
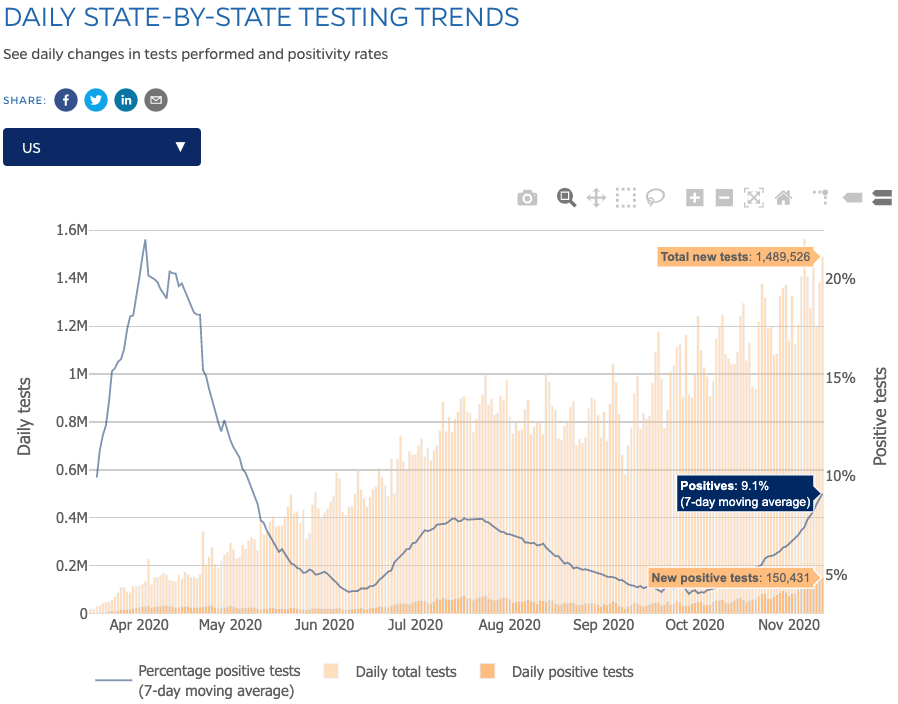
The U.S. is seeing record highs in daily new confirmed coronavirus cases as the pandemic hits the country with full force as the weather cools.
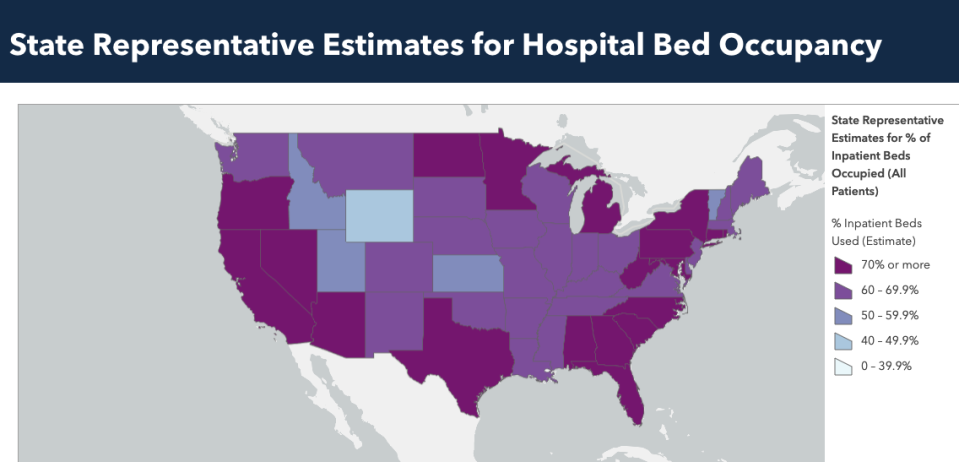
As a result, hospitals are again starting to reach capacity, particularly in ICUs where the most serious patients need to be treated.
Dr. Lakshman Swamy, an ICU physician at Boston Medical Center in Massachusetts, said he and his colleagues are still rationing personal protective equipment (PPE) and reusing N95 masks. Most crucially, as Ed Yong detailed in The Atlantic, hospitals need more able-bodied health care workers.
“We need staff,” Swamy said on Yahoo Finance Live. “How many people had to come in from other regions to help New York, to help Boston? And we need to have those pipelines ready and ready to go, because staff everywhere are still exhausted, and we’re dreading the double, triple shifts, all that stuff that we know is coming.”
‘Of course we’re worried’
In the spring, when most of the country was on lockdown due to stay-at-home mandates, patients began overwhelming hospitals with cases of COVID-19, the disease caused by the coronavirus.
This caused some hospitals to take extraordinary measures, like using portable morgues in vans outside and using trash bags as PPE. Although things would eventually subside in most parts of the country, the spike in cases is indicating that conditions could revert back.
“In the spring, the hospitals were under extreme strain,” Swamy said. “When you hit that point, I think the care that’s delivered is just frayed, fragmented, diluted. It’s hard to give people the attention they need.”
In Texas, where cases topped 1 million this week, the city of El Paso resorted to mobile morgues because of high death count in the city — and the city already needs more trailers.
“What’s especially concerning is that I’m wearing the N95 for the entire shift now,” Swamy said. “Everything is getting a lot more use out of it, and we’re reusing it a lot. But on the other hand, it doesn’t feel like the supply is going to fall out from under our feet like it did so much in the spring. This is all in the setting of rising cases without a real surge still though, so of course we’re worried.”
Although news from Pfizer about its COVID-19 vaccine seeing successful results is a good sign, it likely won’t be available for widespread distribution until at least 2021.

In the meantime, there’s no one simple solution to this second wave, other than to stay at home as much as possible and continue social distancing and face mask measures.
“The most important thing right now is for people to realize that you can get away with doing a lot less in terms of pulling back on indoor dining and all of this without having to do a full lockdown if you do it sooner,” Swamy said, adding: “Individual actions matter too. Just because indoor dining is open doesn’t mean everyone has to go and use it.”
‘COVID absolutely exposes all of the vulnerabilities’
One silver lining for the record surge is that health professionals know more about what they’re dealing with and how to approach treatment.
“The infection is spreading widely in a different way,” Swamy said. “We know what we’re doing better. We certainly don’t know everything, but we’re improved our practices significantly. We’ve published on this a good bit — not intubating quite as early, quite as aggressively, using alternate technologies to get oxygen in without the breathing tube, without the ventilator, dexamethasone, remdesivir. We have more knowledge, more skill now than we did in the spring.”
Over the past year, doctors have learned that hydroxychloroquine is not a proper treatment for the virus, but drugs like dexamethasone and remdesivir are. (President Trump was treated with the two medications after he was hospitalized with the virus back in October.)
Public health experts have also been able to see which communities have been particularly vulnerable to the virus: communities of color. Swamy stressed that it’s essential to use this knowledge to help with treatment going forward.
“COVID absolutely exposes all of the vulnerabilities in our health care system, especially how fragmented and siloed we are within an institution, between institutions, between regions, between states,” he said. “And we’ve advocated for senior leadership at the federal level to say we need to move the resources to where they’re needed, not just ventilators but people.”
Adriana Belmonte is a reporter and editor covering politics and health care policy for Yahoo Finance. You can follow her on Twitter @adrianambells.
READ MORE:
Coronavirus vaccine 'doesn't help us today' as America sees deadly transmission surge
Coronavirus: ‘These attacks on experts are going to haunt us,’ doctor says
Coronavirus: ‘The pandemic is clearly out of control’ and America needs to mask up, doctor warns
Read the latest financial and business news from Yahoo Finance
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, LinkedIn, YouTube, and reddit.