2021 health insurance rates are coming out despite 'unprecedented uncertainty'
Health insurance premium rates are starting to come in for 2021, giving people an idea for what insurance may cost for the first time since the coronavirus crisis began. But not much more than an idea.
The first rates proposed and released to the public — from Vermont, Washington, D.C., and Oregon — provide a glimpse into what health insurance will cost in 2021, but almost every insurance company that referenced the pandemic stressed the unprecedented level of uncertainty for 2021.
Rates are calculated by insurers and proposed to states every spring for the following year, usually with data from the complete year before, which in this case would be 2019. States analyze the rates and decide if they’re fair, and negotiate with insurers if not. Not all states publish proposed rates as they get them from insurers, but usually by August the rates are finalized, collected, and published on the federal government’s website.
Some insurers tried to account for COVID-19 cost projections for 2021, but many admitted that the vast uncertainty surrounding literally every aspect regarding the pandemic adds significant guesswork to estimating next year’s rates.
Insurers are usually prohibited from using losses from the current year as a reason to hike up rates for the next. But that doesn’t mean the COVID-19 crisis can’t be used as a reason if an insurer expects 2021 to be an expensive year.
Actuaries from the Society of Actuaries, which help insurers set rates, said premiums would likely rise between 4% and 6% compared to 2020, without factoring in the pandemic.
The rates trickle in
Vermont’s insurers proposed rates with single-digit increases of 6.3% for Blue Cross Blue Shield of Vermont and 7.3% for MVP, compared to last year’s rates.
MVP said COVID-19 was responsible for 1.6 percentage points of the 7.3%, but Blue Cross Blue Shield of Vermont didn’t mention coronavirus as a factor. The increases are less than 2020's changes, which were in the double-digits, but again, are subject to revision.
Oregon's system saw its six insurance companies providing individual market coverage ranging from a 3.5% decrease to an 11.1% increase for its average premiums. For group coverage, the range was from a 1.1% decrease to a 7.9% increase. The weighted average for individual and group changes would be increases of 2.2% and 3.9%, respectively.
Washington, D.C.’s rates varied considerably. On average in the individual market, CareFirst proposed a 14.7% increase for HMO plans and a decrease of 0.6% for PPO; Kaiser proposed a 2% decrease. For small group plans, Kaiser didn’t have a change, Aetna proposed a 7.4% hike for HMO and a large 38% increase for PPO plans. United proposed increases of 17.4% and 10.3% for its HMO plans and an 11.4% bump for its PPO.
A lot of uncertainty
For rate changes, double-digit jumps are big and single-digit adjustments are typical, and usually represent fairly small dollar-figure increases, unless the plan is particularly pricey. Sometimes the changes are big because of miscalculations in previous years.
But what’s far more interesting is how insurers talk about the future and what they expect the healthcare landscape to look like. Usually, they have a decent idea – but not this time.
Some insurers referenced COVID-19 and some didn’t in their rate proposals to regulators. From the filings, the general picture is that they have no idea what the situation will be and that these are essentially placeholders.
“Insurers are probably just filing what they already would have filed,” said Cynthia Cox of the Kaiser Family Foundation. Some of them, she said, may be factoring things in slightly, but any changes need to be justified to regulators. And without a crystal ball for clarity on 2021 — most analysis is premature.
Even the present is still a mystery, because insurers have enormous gaps of data. The coronavirus crisis is far from over in the U.S. and many of the claims (for hospital treatment, testing) have not been finalized and settled. But even if they had data, that wouldn’t be enough to say much about 2021, when so much rests on full-speed innovation for vaccines and other curative therapies.
“If they had good data about right now it wouldn’t necessarily be representative of a year from now,” said Cox.
As BridgeSpan, an Oregon insurer wrote, “the market is facing unprecedented uncertainty,” and “there is no consensus on the short or long-term impacts of COVID-19.”
Rates are always published in pencil, and states and companies do a lot of erasing, recalculating, and rewriting until things are finalized. But the first draft is especially lightly sketched out this time.
Kaiser wrote, “We do not have any analysis at this time that indicates we should change our rates for 2021, therefore we are not altering our rates for the coronavirus pandemic. It is difficult to say to what extent the coronavirus will have in 2021."
This has been a common theme, but others have baked in small adjustments based on some calculations of potential costs. Cox pointed out that PacificSource, which didn’t adjust for COVID-19, expected costs to be between $0.14 and $35.53 per member per month.
All of this means there will likely be substantial back and forth and adjustments to rates before they’re finalized in August. And after that, it’s possible some insurers will drop out should the situation appear to worsen. Cox said this has happened before, most recently in the early part of the Trump administration when government payments to insurers were in doubt.
The lack of clarity has many layers. A vaccine may come to save the world from coronavirus, but a cure might come first — which might be very expensive even if it’s effective.
“That would drive up costs considerably,” said Cox.
Another layer: Whether elective medical procedures that have been postponed during the crisis will create a wave as patients seek treatment that had been put off.
“That’s another issue that insurers are thinking about,” said Cox. “A lot of knee replacements next year.”
Another assumption some insurers, like MVP in Vermont, has baked into its estimates: a vaccine, costing $75 for 80% of the people the insurer thinks will utilize it. Over 12 months, that is amortized as a $6.25 increase per month.
-
Ethan Wolff-Mann is a writer at Yahoo Finance focusing on consumer issues, personal finance, retail, airlines, and more. Follow him on Twitter @ewolffmann.
McDonald’s to end public soda fountains due to coronavirus pandemic
Insurance premiums expected to rise 4% to 6%, before factoring in COVID
High-yield savings banks finally hit by the Fed's coronavirus rate cut
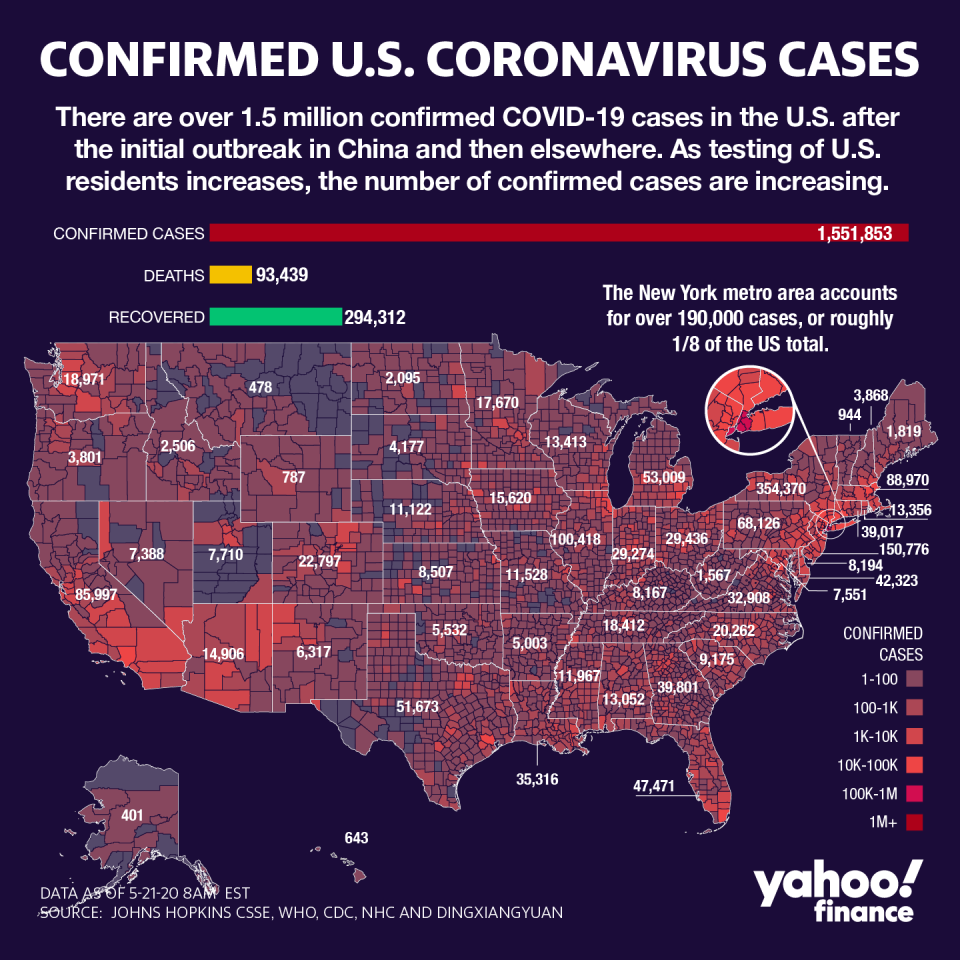
The US may be undercounting COVID-19 cases by a massive margin: Goldman Sachs
Why Amazon, Facebook, Disney saw their chiefs retake control
Why the unemployment rate could be 5 percentage points higher
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, LinkedIn, and YouTube